Faster patient onboarding & care coordination
Secure health record workflows
Reliable telehealth integration


Why Home Healthcare Systems Are Different
Home healthcare systems face challenges that do not exist in centralized care environments. Care delivery is distributed across homes, regions, and care teams, making coordination inherently more complex.
Clinicians, caregivers, administrators, and billing teams all rely on the same underlying systems, but they use them in very different ways. A caregiver needs fast, reliable access in the field. Administrators require visibility across schedules, staffing, and outcomes. Billing teams depend on accuracy and consistency across records and reporting.
Patient and operational data in home healthcare is highly sensitive. Systems must handle this information carefully while still enabling real-time coordination and decision-making. Delays, inconsistencies, or failures can disrupt care delivery and erode trust quickly.
Unlike many business environments, system failures in home healthcare carry a high operational cost. Missed visits, incorrect information, or delayed reporting affect both patient outcomes and organizational stability.
These realities require a level of rigor and systems thinking that goes beyond standard business software.
Home Health Care Digital Solutions
CRMs, schedulers, CMS platforms, EHRs, and EMRs rarely match your unique business logic. When workflows break or teams rely on spreadsheets, it’s time for custom solutions that eliminate complexity and unify operations.
Struggling to scale output?
This speaks directly to growth constraints and system limits, which is a primary driver for custom software.
Tech integration challenges?
Clearly connects to Firestitch’s strength in integrations and custom systems, so it’s very on-brand.
Productivity going down?
Addresses day-to-day operational pain and manual work, which resonates strongly with home health teams.
Common Software Used in Home Health Care
CRMs, schedulers, CMS platforms, EHRs, and EMRs rarely match your unique business logic. When workflows break or teams rely on spreadsheets, it’s time for custom solutions that eliminate complexity and unify operations.
Struggling to scale output?
Your business is growing, but your existing systems can't keep up.
Tech integration challenges?
You find it hard to integrate new technologies into your existing systems.
Launching new services?
You're expanding your services and need tailored tools to support your unique offerings.
Too many mistakes?
Manual errors are becoming a common occurrence.
Why Off-the-Shelf Software Fails Health Care Business
One-Size-Fits-All Doesn't Fit
Generic scheduling software can't handle clinician licensing requirements, patient care protocols, shift continuity, and HIPAA compliance needs.
Data Silos Cost You Money
When patient records, billing, and caregiver scheduling are separate systems, care quality suffers and billing errors multiply.
Manual Workarounds Waste Time
Clinical staff waste hours on manual coordination instead of focusing on patient care quality and outcomes.
Scaling Creates Complexity
Every new patient or clinician creates exponential coordination challenges that increase administrative burden and clinical risk.
Common System Challenges in Home Healthcare
Many home healthcare organizations struggle with systems that were never designed to work together.
Electronic medical records, billing platforms, scheduling tools, and reporting systems often operate in silos. Data must be manually entered or reconciled between systems, increasing the risk of errors and delays. Teams spend time managing process instead of focusing on care delivery and improvement.
Visibility is another persistent challenge. Leaders lack real-time insight into patient status, staff activity, and operational performance. Reporting becomes reactive rather than actionable, especially across multiple locations or services
As organizations scale, these problems intensify. Adding new regions or programs increases complexity, while compliance pressure grows alongside volume. Without intentional architecture, risk increases at the same rate as growth.
Inconsistent reporting and unreliable data undermine confidence across the organization. These are the signals that systems are no longer supporting operations effectively.
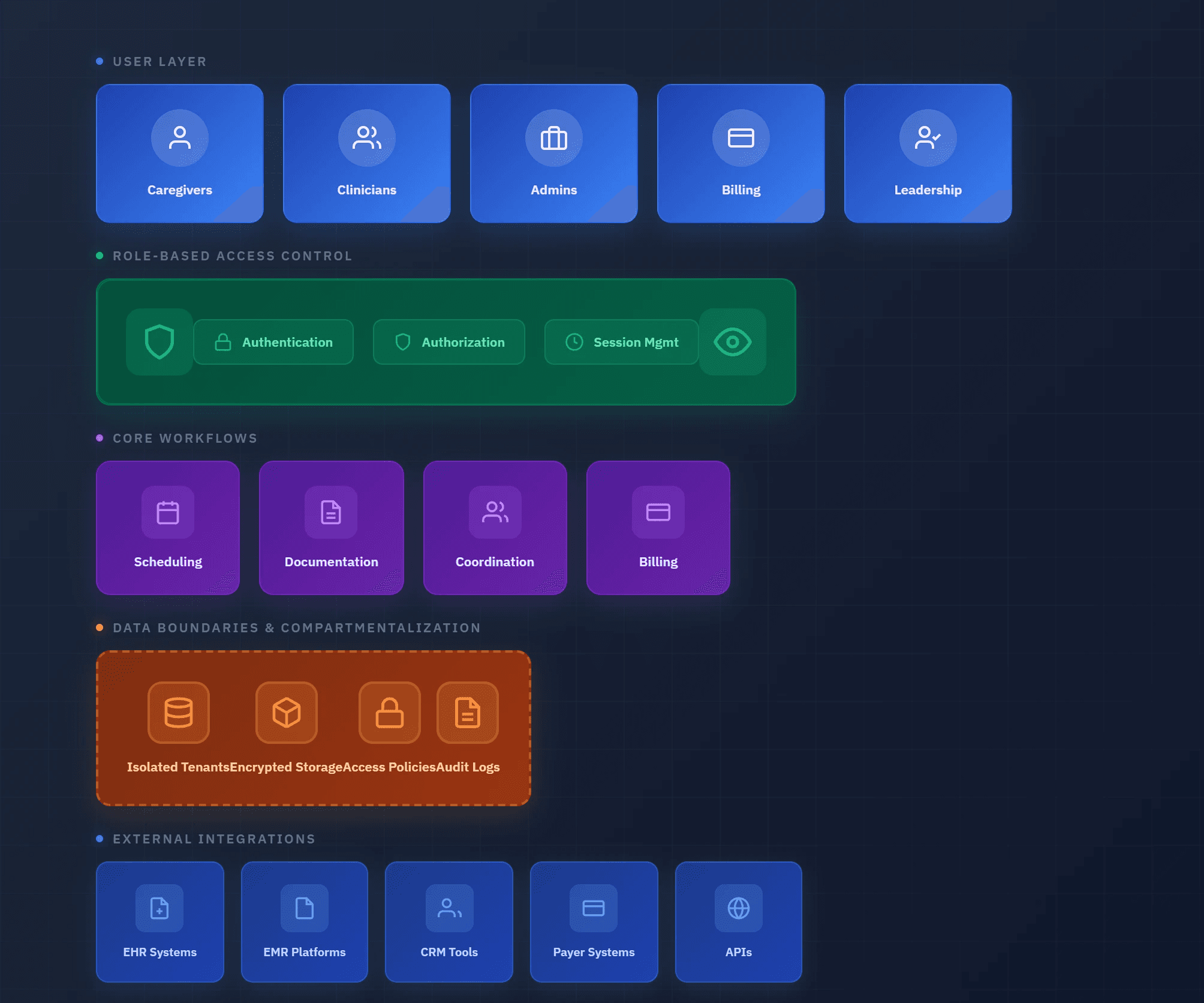
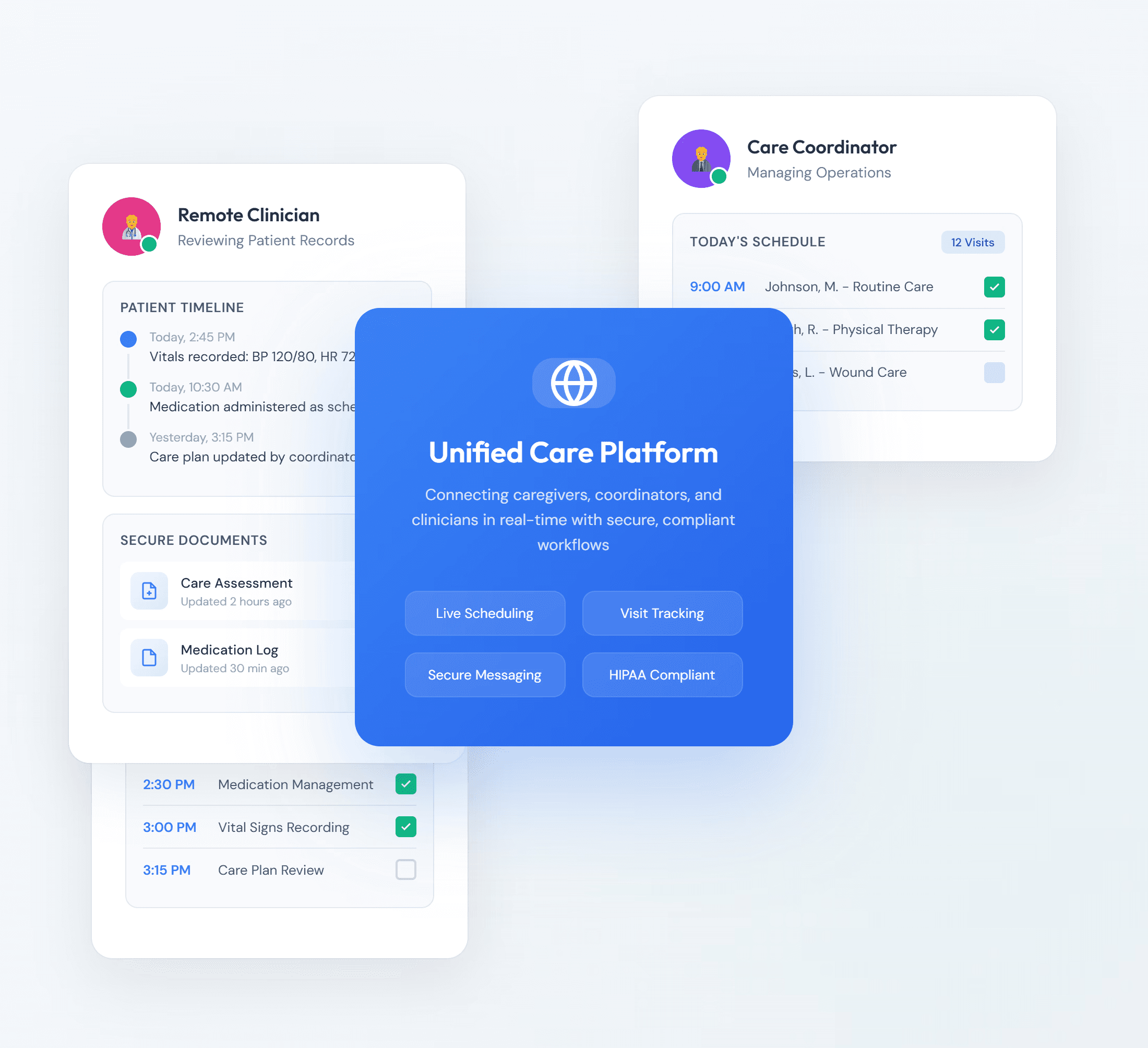
FireStitch approaches home healthcare systems with a systems-first architecture. We design platforms by understanding how data, workflows, and roles interact across the organization.
We design with compliance in mind without positioning ourselves as compliance authorities. Systems are structured to support access control, auditability, and data boundaries so organizations can meet regulatory expectations without constraining operations.
Role-based access ensures clinicians, administrators, leadership, and billing teams see only what they need to perform their responsibilities effectively. This reduces friction while maintaining accountability.
Data minimization and compartmentalization are core principles. Sensitive information is isolated where appropriate to reduce exposure and downstream risk.
Reliability and observability are built into the system. We design platforms so teams know when something breaks, where it broke, and how to respond. This prevents silent failures and supports stable operations at scale.
Relevant Solutions for Home Healthcare Organizations
FireStitch services are applied by outcome, not as disconnected offerings.
Operational Systems
Custom web applications form the operational backbone that revenue depends on. FireStitch builds systems that replace fragmented tools with a single, reliable source of truth across sales, operations, and leadership.
Typical operational systems include:
Scheduling and capacity management platforms that align demand with available resources
Customer and account management systems that unify sales activity, onboarding, and ongoing engagement
Order, fulfillment, or service workflows that reduce handoffs and delays
Internal dashboards that surface real-time operational and revenue signals
These systems are designed to integrate directly with existing CRMs, billing platforms, analytics tools, and third-party services eliminating manual reconciliation and duplicate data entry.
The result is faster execution, fewer dropped handoffs, and clearer ownership across teams. Sales can close with confidence, operations can deliver predictably, and leadership gains visibility into what is happening as it happens.
Organizations typically see:
Shorter sales-to-delivery cycles
Fewer operational bottlenecks as volume increases
More accurate forecasting and reporting
Reduced reliance on spreadsheets and manual coordination
Operational systems stop being a constraint on revenue and start becoming an enabler of growth.
Mobile Access for Field Teams
Field teams operate in environments where time, connectivity, and accuracy matter. FireStitch builds mobile applications that give caregivers and clinicians reliable access to the information they need while working in homes, facilities, and in transit.
For home healthcare organizations like Lumacare, mobile tools are not optional they are the primary interface between care delivery and the underlying system.
Typical mobile solutions include:
Visit management applications that surface schedules, patient context, and care tasks in one place
In-field documentation tools that allow clinicians to complete notes, forms, and confirmations at the point of care
Offline-capable workflows that continue functioning in low-connectivity environments and sync automatically when a connection is restored
Secure access controls that ensure sensitive information is only available to authorized roles
These applications integrate directly with operational systems, scheduling platforms, and reporting tools, eliminating the need for double entry or post-visit administrative work.
For organizations like Lumacare, this results in fewer missed or delayed visits, faster documentation completion, and improved accuracy across clinical and operational data. Care teams spend less time navigating systems and more time focused on care delivery.
Leadership gains clearer visibility into field activity in real time, while clinicians experience tools that feel supportive rather than obstructive.
Mobile access becomes a stabilizing force for distributed operations not a source of friction.
Automation and Visibility
Workflow automation and visibility only create value when they reflect how work actually moves through the organization. FireStitch designs automation that reduces manual handoffs and surfaces the operational signals that matter before issues compound.
Automation is applied to real processes, including:
Intake and request workflows that route work automatically based on role, capacity, or priority
Approvals and handoffs that enforce accountability without relying on email or tribal knowledge
Status transitions that update downstream systems the moment work progresses
Exception handling that flags delays, missing data, or failed steps immediately
These workflows feed directly into live operational dashboards not static reports.
Dashboards are designed around decisions, not vanity metrics. Leaders see:
Work in progress vs. stalled work
Capacity and throughput by team or region
Bottlenecks that are slowing delivery or revenue recognition
Signals that indicate risk before outcomes are affected
Field teams and operators see clear task state, next steps, and confirmation that actions were completed successfully.
Metrics are transparent, shared, and derived from system behavior not manual reporting. When something breaks or slows down, the system makes it visible in real time so teams can respond immediately.
Automation and visibility together shift operations from reactive to controlled, allowing growth without losing clarity or accountability.
Data and Integrations
Modern operations depend on systems working together reliably. FireStitch designs integrations that connect core platforms so data moves automatically, consistently, and predictably across the organization.
In regulated and operationally complex environments, this often includes integrating:
EHR and EMR systems that manage clinical records and care documentation
Scheduling and visit management platforms that coordinate staff, locations, and capacity
Billing and financial systems that track services delivered, claims, and revenue recognition
CRM and intake systems that manage referrals, customers, and ongoing relationships
Patient or customer portals that provide access to schedules, documents, and communication
These systems are rarely designed to work together out of the box. FireStitch builds secure, purpose-driven integrations that ensure data is entered once and reused everywhere it is needed.
Events in one system trigger updates across others automatically. A completed visit updates documentation, billing, and reporting. A scheduling change is reflected immediately in mobile tools, dashboards, and notifications. Intake data flows cleanly into operational and clinical workflows without manual re-entry.
Data integrity is prioritized. Integrations are designed with validation, error handling, and monitoring so failures are visible and recoverable rather than silent. Teams know when something breaks and why.
The result is a connected system where operations, care delivery, and leadership all rely on the same information. Manual reconciliation disappears, reporting becomes trustworthy, and teams spend time acting instead of fixing data.
Integrations stop being fragile dependencies and become a stable foundation for scale.
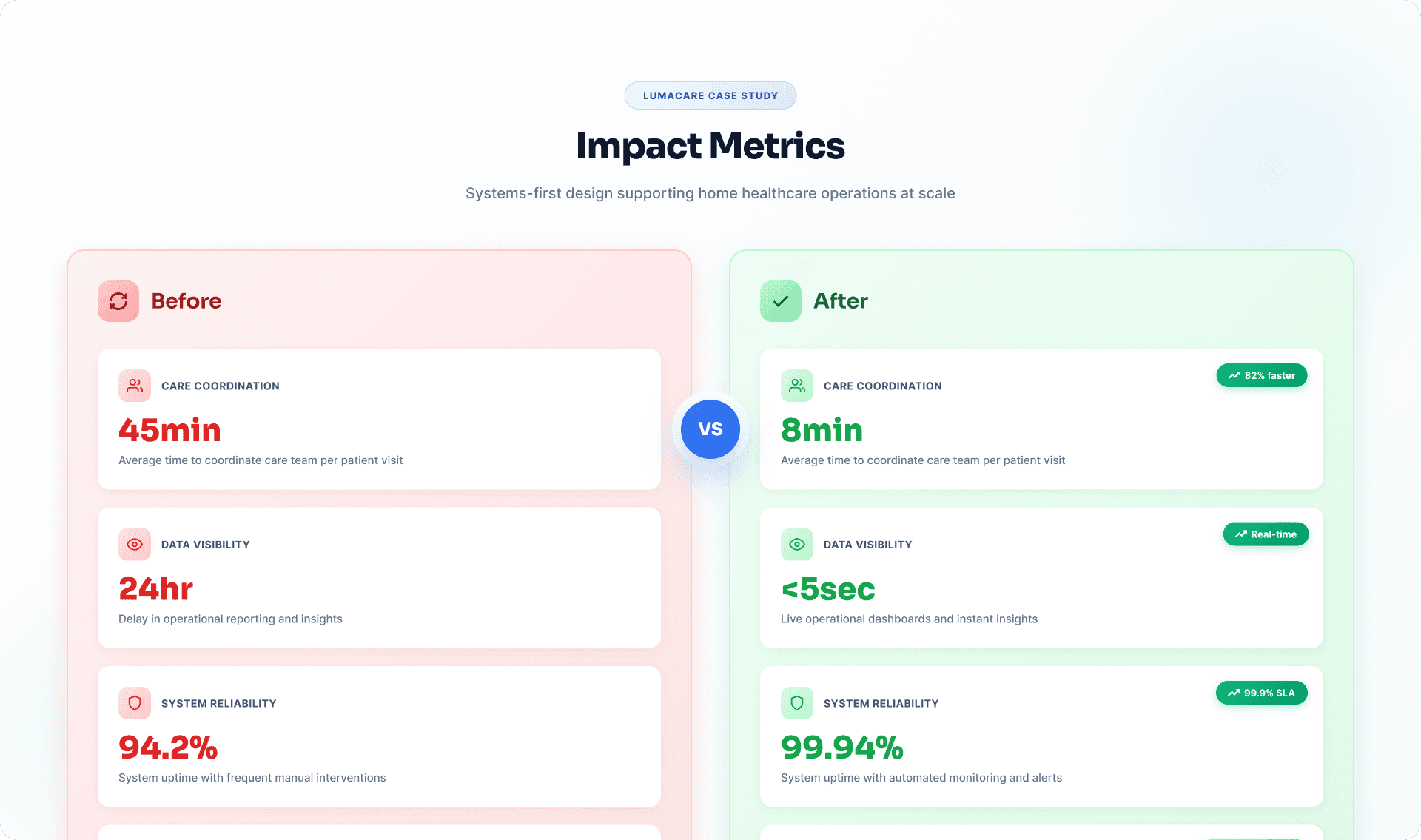
FireStitch’s work with organizations like Lumacare demonstrates how systems-first design supports home healthcare operations at scale.
In this engagement, FireStitch helped modernize systems that support care coordination, data visibility, and operational reliability. The focus was not just on building features, but on creating systems that teams could trust as volume and complexity increased.
When Home Healthcare Organizations Typically Engage FireStitch
Home healthcare organizations often engage FireStitch when:
1
Expanding into new regions or service lines
2
Replacing spreadsheets and manual coordination processes
3
Preparing for audits or increased compliance scrutiny
4
Leadership no longer trusts reporting or operational data
5
Legacy systems are limiting growth or adaptability
Related Insights and Resources
Explore related content to deepen your understanding of how systems support home healthcare operations:
1
Healthcare systems and regulated data articles
2
Workflow automation insights
3
Systems integration and API strategy posts
4
UX and architecture content for complex applications
These resources strengthen internal context and support informed decision-making.
FireStitch Case Studies
Explore real projects and outcomes that show how our toolkit helps teams ship intuitive, industry-ready solutions faster and smarter.
Frequently Asked Questions
What is home health care software development?
Can you integrate home health systems with CRMs?
What home health workflows do you build?
Can you improve caregiver scheduling and reduce manual errors?
How do you approach HIPAA-conscious workflows?
Book FireStitch Office Hours
FireStitch Office Hours are free, one-on-one strategy sessions with FireStitch CEO Keith Seim and senior FireStitch strategists. These sessions are not sales calls. They are working conversations designed to help us understand your business, review your current systems, surface bottlenecks, and talk through realistic paths forward. The goal is simple: clarity. You’ll walk away with a better understanding of what’s holding you back, what’s possible next, and whether FireStitch is the right fit to help you get there no obligation either way.